|
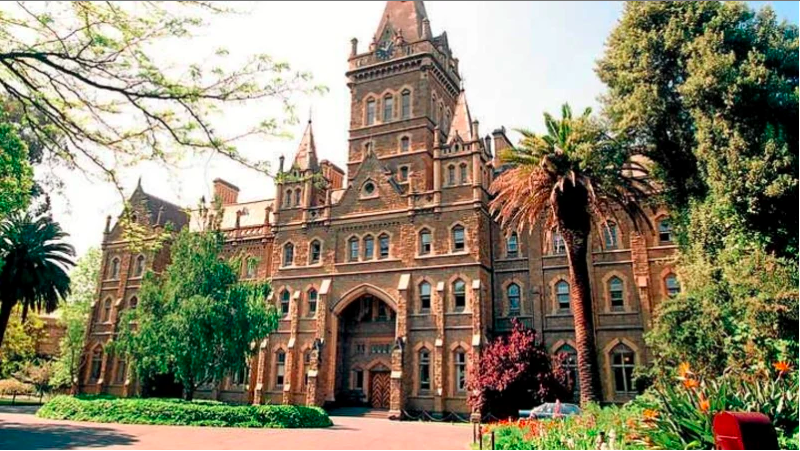
On to the main part of our trip, meetings. With the help of Dr. Andreia Bruno, we were able to book the “Hercules Room” at Monash University-Parkville Campus. Fully equipped with Zoom capable screens and secret cabinets of food and drinks, student leaders discussed not only different projects but also the sustainability and leadership of PharmAlliance student domain. UNC leaders (Clara Kim, Vraj Patel, Jenny Jin, Ember Lu) and Monash University leaders (Alisha Cloti, Kevin Wu, Brandon Pham) were in attendance, while Ruby Akkad from UCL called in from Toronto due to last minute visa issues.
This was the first time that student leaders were able to meet in person. We realized that the value of this face-to-face communication is vital, as the quality of the conversation was much higher and we were able to accomplish much more action items and structures. Ember and I had created meeting agenda templates beforehand, and each school was in charge of different sections of the meeting. Everyone created agendas before their meeting and came well prepared to host the meeting and guide discussions. The first day was spent mostly discussing PharmAlliance student domain leadership so far. The leaders first drafted a mission statement of PharmAlliance student domain: While aligning with initiatives on the PharmAlliance level at the highest possible extent, collaborate on impactful and challenging pharmacy issues that are common between the US, Australia, and the UK. Then, students discussed about different issues with leadership that came up in effectively leading organizations. Students were able to share their experiences and also give advice on how to overcome obstacles. The next day was spent on discussing the Medication Safety Comic series. We decided on logistics, themes, and different topics we want to be included in the comic series. While discussing all of the topics, we made sure that our end goal was having an element of collaboration in each step. Collaboration sometimes may be inefficient; In fact, there are tasks that could easily be done if it were just done within one campus group. However, the leaders were eager to implement collaborative portions across the project, as that is the main goal of PharmAlliance itself. Also, students and leaders in PharmAlliance truly value the unique international collaboration we are fortunate to be a part of, and wanted to take full advantage. The last day was spent discussion the International Case Competition. Vraj Patel and Brandon Pham led the discussions on assessing what was good versus what could be better compared to last year. At the end of the meeting, the leadership team decided to make create interschool teams - i.e. each team will have students from two different countries! This was an exciting development compared to last year, where teams were composed of students in one school. This was again a decision made with the desire to increase collaboration among students across all three countries. We hope that the International Case Competition becomes a unique opportunity for students to learn about each others’ pharmacy practices.
2 Comments
A group of Pharm.D. students received a $10,000 PharmAlliance grant — the first of its kind to be awarded to Pharm.D. students — to support a project promoting medication safety. The project is led by PY3 Clara Kim and PY2 Vraj Patel from the UNC Eshelman School of Pharmacy. It is co-authored by PY3 Ember Lu from the School and students from University College London and Monash University in Melbourne, Australia. Their initiative aims to promote safe use of the three medications most associated with drug errors — opioids, insulins and anticoagulants — through the creation of a comic series that promotes patient education. The comics will be distributed online through social media and offline as posters and fliers posted in community pharmacies in the U.S., England and Australia. “This project will help patients, including those with low health literacy, understand how to take their medications correctly and acknowledge the importance of adherence, while making it fun in the process,” Kim said. Established in 2015, PharmAlliance is an international partnership between the UNC Eshelman School of Pharmacy, University College London and Monash University. PharmAlliance has provided support for research initiatives developed by faculty and Ph.D. students from each of the three schools. This is the first PharmAlliance grant to be awarded to Pharm.D. students. Along with Kim, Patel and Lu, the project’s co-authors include Monash University students Alisha Cloti and Emma Hatherley, and University College of London student Ruby Akkad. “The student leaders of all three schools are very excited and thankful to be the first student group to have received this grant,” Kim said. “This is a very important step for the PharmAlliance student domain.” The students will be mentored by faculty at each school: David Steeb, Pharm.D., M.P.H. at UNC-Chapel Hill, Andreia Bruno, Ph.D. at Monash University, and Oksana Pyzik, M.Pharm. at UCL. The grant will allow the students to develop their project beyond the conceptual stage and travel to Melbourne to discuss their project, as well as ways PharmAlliance can support student initiatives and foster connections between students at each of the schools in the future. Original article found here, published on November 13, 2018 at the UNC Eshelman School of Pharmacy homepage:
Continuing on from last week, this time we will covering part time work experiences from students working in hospital and community pharmacies. Community- Chemist Warehouse - 2nd year pharmacy student Chemist Warehouse is a very large community pharmacy chain in Australia. So, in a company so large, I thought that the service provided might be more impersonal than a private pharmacy. I couldn’t have been more wrong. I can’t speak for every store, but at my pharmacy it’s commonplace to know all of the regular customers by name. Our priority is putting the health and wellbeing of the customer first, and this is prioritised over selling them products that they might not need. All of the staff, including the pharmacy assistants, are trained in co-therapy. This means that the pharmacist can direct patients to the pharmacy assistants, where any additional products needed to combat side effects (or to supplement their therapy) can be recommended. Working as a student has helped me in so many ways. Working also allows me to see real life cases and scenarios, and to be involved in problem-solving when our pharmacy receives an atypical script or patient. Working has also helped me to develop my counselling skills, as well as my dispensing and drug knowledge. I mentioned earlier that our staff is all trained in co-therapy and S2 products; at university, I can apply my knowledge of these products in the non-pharmacological section of my counselling. So, my university studies help me at work, and my knowledge from work helps me at university. For any student looking to advance their knowledge and practical skills, I would recommend starting a job at a community pharmacy. The training and effort that they put into their pharmacy students has really benefited me and I've found it really valuable. I hope this helps shed a little light onto what working in a community pharmacy is like. In this 2 part blog post, we have compiled student experiences from students who went on exchange to Malaysia and also from 3 pharmacy students each representing the 3 main types of pharmacies in Australia: compounding, community and hospital pharmacies.
This week, we will focus on the exchange experiences and compounding pharmacy part time work. Have a read below and find out more about what it's like to work in the various types of pharmacies we have in Australia and their similarities/ differences! Visit the blog again next week to read about part time work experiences in community and hospital pharmacies! Considering the fact media these days are constantly badgering society about the health impacts of obesity and our ever-increasing sedentary lifestyles, it should not have come as a shock that a high proportion of the top drugs used by Australians are all cardiovascular related. Combine that with the problematic over-prescribing of common antibiotics and the ever rising prevalence of type two diabetes, and the top 10 medications shouldn’t really have been too hard to guess either.
When looking at the most commonly used drugs within Australia, there were two ways to go about it; Either purely by the number of prescriptions filled for that particular medication each year, or more specifically the number of individuals per 1000 people who take a standardised dose of this medication each day. Looking directly at the number of prescriptions, it is clear that as a nation we are battling with hypercholesterolemia in high numbers. With over ten million prescriptions filled for both atorvastatin and rosuvastatin, they each claim the gold and silver medals respectively at the top of our list. Not only this, but when comparing these drugs with lists from the previous year, yet again they were highly featured with atorvastatin remaining as number one and rosuvastatin claiming third, showing a trend which can be traced back for a number of years. To fill out the top three by prescription numbers from July 2016-June 2017, esomeprazole took the bronze with around six and a half million scripts filled within the twelve month period. Whilst this was a drop from second place during the previous year, the notably high positions of both itself and its fellow proton-pump inhibitor pantoprazole (fourth place, up from fifth the previous year) shows that conditions such as GERD and gastric ulcers are becoming more and more prevalent amongst the community. Whether this can be associated with an increase in the self-use of OTC anti-inflammatories, or an increase in fatty or spicy foods within the diets of Australians may be up for speculation, however the numbers speak for themselves. Rounding out the top ten by prescription count are commonly prescribed antibiotics such as amoxicillin and cephalexin, as well as medications for blood pressure and diabetes. However, some observations that can be made from this list are the high number of antibiotic scripts being filled within Australia. With the total count of the top three exceeding fifteen million, it is clear that a high proportion of Australians have undergone courses of antibiotics under the recommendation of doctors, especially considering the population of Australia currently sits at around 24 million people. On the other hand, when analysing the medications used by the Australian population, the best measure to gain some perspective on the number of people taking drugs for chronic conditions is to look at the number of individuals per 1000 people who take a standard daily of dose of a specific medication. And when looking at the list, the prevalence of cardiovascular conditions such as hypertension and hypercholesterolemia are huge, with eight of the top ten medications coming under the umbrella of cardiovascular medications. And once again taking the top two spots, and not surprisingly after our previous list, were HMG-CoA reductase inhibitors atorvastatin and rosuvastatin. Not only are these drugs considered highly effective at lowering patient’s cholesterol levels, but they are also very easily accessed due to their relative low price point. Not only that, but their positive effects are easily monitored by doctors through a simple blood test. Rounding out the top three within Australia was perindopril, an ACE inhibitor commonly prescribed for the lowering of blood pressure, as well as for patients with established coronary heart disease in order to lower the risk of a myocardial infarction. And while it is a first line therapy choice for patients with hypertension, it also needs to be monitored carefully, particularly amongst patients taking diuretics or NSAIDs. This is due to what we call the ‘triple whammy effect’ which actually reduces the effectiveness of the ACE inhibitor in controlling a patient’s blood pressure. However, like the statins, perindopril is also an easy to access medication with relatively low prices. Now when compiling this list there are some medications which were not counted, presumably as they are not covered by the Pharmaceutical Benefits Scheme, and in fact cheaper to purchase over the counter without a script or even simply more convenient. So, whilst there are a large number of patients regularly taking high dose paracetamol in order to control pain, and there are large numbers of salbutamol inhalers being sold daily within pharmacies around the country in order to control asthma symptoms, they are not shown as part of these statistics. When looking at the drugs that are regularly used by Australians it is clear that our cardiovascular health is deteriorating as a nation. If a prediction was to be made about future lists and medication use for the years to come, we could probably say that these figures are unlikely to change a lot as well. But if one thing is for sure, it is that with the ever increasing demand of medication usage in Australia, the need for helpful and involved pharmacists is as high as ever. Figures and statistics obtained from The Commonwealth of Australia’s Department of Health and published on NPS Medicine Wise. Links to the top drug tables from both 2016-17 and 2015-16 can be found below. Top Drugs in Australia 2016-2017-https://www.nps.org.au/australian-prescriber/articles/top-10-drugs-2016-17 Top Drugs in Australia 2015-2016-https://www.nps.org.au/australian-prescriber/articles/top-10-drugs-2015-16 At Monash, we experience 4 kinds of pharmacy placements. A little about each type of placement has been written by some Monash students including Pharmalliance committee members Alisha and Emma. Read ahead to find out their experiences from their January/ February placements!
1. Community: Students spend 3 weeks gaining practical experience in a local pharmacy where they learn to dispense and counsel on medications and provide health education to the general public. Students can choose to do 1 or 2 community placements. 2. Hospital: Students get 2 opportunities throughout the year to work in major hospitals in Melbourne. In here, we get a chance to work in a multidisciplinary team and contribute in treating patients with complex health conditions as well as dispensing prescriptions and observe sterile manufacturing.These placements last for 3 weeks as well. This is how my friend, Krista, found it. I remember being very nervous and apprehensive about going to my very first hospital placement. I believe everything ran smoothly due to the great organisation skills of the PEP (Professional Experience Placement) staff. It was a relief that the PEP staff took into account our residential addresses when allocating us to our hospital locations. I was allocated to complete my placement at Sunshine Hospital which was less than an hour’s worth of commuting, of which I was very grateful. The pharmacy department staff were very accommodating and welcoming. They certainly went above and beyond to ensure that we felt comfortable. Our preceptor Dorothy, was so helpful and genuinely cared for our well-being and education. She was very organised and allocated us timetables to various wards to make sure we were exposed to as much of the hospital as possible. She would even take the time out of her day to meet us for daily education sessions. We found these sessions so helpful and handy and we will never forget how awesome she made our first hospital placement to be. 3. Rural: Students have a choice to go to a rural town to participate in activities in a community pharmacy of that area and in some cases, work in a rural hospital. This placement not only trains us to be pharmacists but also demonstrates the rural lifestyle and its challenges. 4. Remote Rural: I was lucky enough have the opportunity to visit a remote area of Australia for 6 weeks. It did take up part of my summer holidays but coming to Broken Hill, a mining town in the Outback, gave me a chance to learn of the positive and negative aspects of healthcare in remote areas of Australia. Visiting Broken Hill provided me experience in a community pharmacy and in a remote hospital where healthcare workers must overcome challenges due to their location to provide their patients the best treatment possible. I’ve learned how mining affects the health of the locals and of the programs in place to enhance Aboriginal health (such as Close the Gap). The locals in Broken Hill are friendly but a stoic bunch as they have endured droughts and floods of the desert. Some patients live or work in isolated areas such as the sheep station we visited. This is why healthcare in a remote area requires specialised services such as the Royal Flying Doctors Service to fly some patients to the Broken Hill hospital or to more specialised centres in cities. In some cases, an offroads ambulance is required to drive to areas where the airplanes can’t land. I guess you can say that there’s never a dull day with healthcare in Broken Hill! Pharmacy education at Monash Currently at Monash, our degree pathway is changing. When I began university, I entered the Bachelors of Pharmacy straight after completing high school. This degree is 4 years long and incorporates theory and practical components to prepare us for our future career. Students must work as an intern in either a hospital or community pharmacy to gain additional practice experience in the healthcare world to qualify as a practicing pharmacist. After this, they complete the pharmacy board registration exam to practice as a licensed pharmacist. Beginning in 2017, the course of study shifted to a Bachelor of Pharmacy (Honours) /Masters of Pharmacy which students can still enter directly after completing high school but is now a 5 year program. For the 2017 student cohort and onwards, the intern year is incorporated into their degree instead of at the end of the 4 year degree. Education in pharmacy covers a broad range of topics from physics to ethics as the role of a pharmacist is and must be very flexible. At Monash, we have lectures and lab sessions. We even grow bacteria! There are also practical components where students are encouraged to learn how to practice in real life situations. For example, we have OSCE role plays, tutorials with experienced pharmacists, and practical learning through placements in hospitals or community pharmacies. Pharmacy education at UNC ESoP Here at UNC ESoP, students can start applying for pharmacy school as early as their sophomore year of undergraduate studies. Upon submitting all the requirements, selected students are invited to the school for an interview process, also known as candidate’s day at UNC ESoP. UNC ESoP has recently transitioned from traditional interviews to Mini Multiple Interviews (MMI), which consist of seven stations where students have a limited amount of time to discuss the topic for that specific station. Classes at UNC ESoP are organized to help students develop a strong foundation and basic understanding of pharmacy before branching out to take various elective courses, followed by the final 4th year rotation called APPE. With the mindset that the greatest learning curve occurs when students apply their knowledge, UNC ESoP designed the early immersion program that allows students to gain hands-on experience as early as the summer after their first year in pharmacy school, also known as IPPE. IPPE divided into three different immersion experiences spread throughout the first three years of pharmacy school consisting of Health System, Community, and Direct Patient Care Experience. Finally, after all of these experiences, there’s only one other thing left between us and graduating with our Doctorate of Pharmacy (Pharm.D.) degree, which is the North American Pharmacist Licensure Examination (NAPLEX) that every pharmacy student must pass in order to get their pharmacy license. Once completed, students may continue on their pharmacy career path to either apply for pharmacy positions, residency, fellowships, etc. with their Pharm.D. degree. On behalf of UNC ESoP pharmily, I am sending our warmest greetings from the US! Pharmacy education at UCL In the United Kingdom, all students wishing to register as a pharmacist must study the four-year Master of Pharmacy (MPharm.) program. The MPharm. program at UCL gives students an exciting opportunity to study aspects of chemistry and biology: integrating academic knowledge with clinical concepts in order to provide better patient care. During four years of study at university, the central theme is preparing students for practice by taking a holistic approach to education. The course each year is roughly split into four areas. Students study courses in pharmacy practice, chemistry, formulation science and biology using a variety of different teaching styles and methods such as lectures, practicals, tutorials, workshops and seminars. Concepts become more complex with progression through the course with rigorous academic work as part of the student experience. That is being said, the course is rewarding albeit challenging, and keeps the idea of a patient at the heart of all study. Following graduation, each student must complete a 52-week placement in a clinical environment. Upon completion of the placement, students must sit for a final exam regulated by the General Pharmaceutical Council. Successfully passing this exam will allow students to join the register as a fully qualified, practicing pharmacist. |
�
Categories
All
Archives
October 2022
|